Focus on the perilous ‘trip’ of K-Land/K-Hole
Ketamine was introduced by Calvin Stevens in 1962 and since then it found a firm place in clinical anaesthesia. It has unique properties as compared with other anaesthetics as it can be given intravenously, intramuscularly, orally and via other routes. Moreover, haemodynamic stability is maintained when ketamine being used and is a preferred anaesthetic while managing a shocked patient. In this article Dr Sher Mohammad and others look at the effects experienced of the dissociative anaesthetic ketamine.
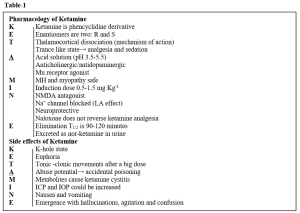
The pharmacology is briefly outlined in table-1
Why Ketamine is a popular recreational drug
Unfortunately, since the 1980s, this drug has been abused as a recreational drug in night clubs and house parties. Its popularity has increased tremendously because it has been erroneously believed to be safer than other recreational drugs. It is available in white powder, tablet or capsule form. When inhaled through the nostril, its effects appear after 10 minutes. The psychedelic experience (‘trip’) includes the sensations of light throughout the body, sensation of being weightless and floating or hovering, colourful visions and out of body experience. The bulk of a ‘trip’ lasts for about an hour and the effects diminish gradually over another hour. This is the experience that the addicts crave for.
What is K-Land and K-Hole
K-Land refers to the effects experienced at low doses of ketamine. The abuser may feel euphoric and experience mild dissociation, where s/he feels slightly detached from reality and the surroundings, but still have some bodily control and environmental awareness. Mellow and colourful experiences(K-land), sink into a blissful infantile inertia (Baby food) and believe that s/he has met the God, are the descriptions.
K-Hole means feeling of falling into a hole or stuck in a hole and it refers to an intense dissociative state caused by a high dose of ketamine. In this state, people may feel completely disconnected from their body or surroundings. Research has shown that this phenomenon occurs due to ketamine’s strong antagonistic effect on NMDA receptors in the brain. Some report out-of-body experiences, while others describe it as entering a void [1].
When someone has “fallen into K-hole”, they are temporarily unable to interact with others or the world around. It is a state between intoxication and coma.
The K-Hole is typically considered undesirable and frequently occurs due to accidental overdose, but occasionally the abusers will consider the experience of K-holing spiritually or recreationally valuable. The high dosages of ketamine necessary to induce a K-hole are unsafe and carry significant physical and psychological risks associated with both acute toxicity and chronic exposure.[2]
Why Does the K-Hole Happen?
Ketamine is a dissociative anaesthetic that fundamentally alters neural connectivity patterns [3]. Studies indicate that ketamine disrupts the default mode network, leading to altered states of consciousness [4]. The acute effects of ketamine vary by dose, setting, and individual biology. In recreational settings, people often take too much or mix substances—raising the risk of slipping into a K-hole.
Ketamine is also used in the Management of Treatment-resistant depression
Ketamine and esketamine represent a significant advancement in the management of treatment-resistant depression and acute suicidality, offering rapid antidepressant effects through glutamatergic modulation and enhancement of synaptic plasticity, rather than traditional monoaminergic pathways [5][6]. However, their use is associated with important risks, including transient dissociation, psychotomimetic symptoms, and potential for abuse, which necessitate careful patient selection and monitoring [7][8][9].
Recreational usage
Ketamine recreational users have found great appeal in its antidepressant, dissociative and hallucinatory effects that are characteristic of the K-hole experience [10]. Whereas the common recreational dose of ketamine is approximately 30–75 mg, a dose of more than 150 mg is required to enter the K-hole[11].
Timeline of effects:
It is to be remembered that everyone reacts differently. One may feel the effects sooner or later than others. Generally, the effects of ketamine kick in within:
- Sixty seconds if injected as we see it being used as an induction agent during GA
- Five to fifteen minutes if snorted
- Thirty minutes if taken orally
The intensity and length are influenced by the users’ current mental state, previous experience and drug dosage [12]. During K-hole, users experience a high level of detachment from the environment, resulting in an inability to respond to surroundings and move their bodies functionally [13]. A high number of recreational users report that the most appealing effects of this experience are “melting into surroundings”, “visual hallucinations”, “out of body experience” and “giggliness*”.
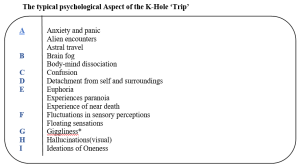
The features of K-HOLE are outlined as follow.
*Giggly: laughing in a silly, childlike, often uncontrollable way due to amusement, nervousness or embarrassment
Physical effects of K-HOLING
By contrast, the least frequent and most negative effects include near-death experiences[12] and physical health problems, like the so-called “K-cramps” from gastric pain, bladder failure, and unappealing mental side-effects, like “memory loss“. “Decreased sociability” are also reported post-K-hole.
Despite its addictive risks, ketamine is considered by many to be “harmless” and thus a “drug of choice”[12] Recreational users seem to be in discord about the K-hole. Many individuals describe it as a fascinating life-changing experience and a spiritual journey resulting in some form of spiritual realization. They state that this experience provided clairvoyance** and assisted them to get through mental disorders like depression and social anxiety[14].
**Clair means clear, voir means to see. The supposed faculty of perceiving things or events in the future or beyond normal sensory contact.
Risks
Frequent K-hole experiences can also result in episodic and semantic memory impairments[15] Depending on how long this state lasts, hallucinations and symptoms of psychosis can develop[16]. The K-hole experience can produce physical risks. For instance, bladder damage can be an indication of ketamine-induced (ulcerative) interstitial cystitis[17],[18].
Contributors to undesirable experiences
Like all psychedelic experiences, there are many factors-particularly” set and settings” that contribute to positive or negative experience. Because K-hole often occurs during clinically unsupervised recreational use, individuals may find themselves in less than favourable circumstances.
- Adequate medical support not available
- Crowded public settings
- Cocktail of ketamine with alcohol or illicit drugs
- Dehydration
- General unpreparedness for the intensity of the experience.
How to Help a victim of K-Hole at the Scene
Once a victim of K-hole is spotted, it is crucial to stay with the person until medical help arrives, monitoring their breathing closely as respiratory depression is a common risk.
Handle the individual carefully, as agitation or hallucinations are common.
Hospital Management
If the individual is unresponsive, follow ABCD
Airway: Make sure the airway is clear.
Position the person to keep the airway open, such as recovery position
Breathing: Look, listen, and feel for signs of breathing.
If the person isn’t breathing, start with bag mask ventilation
Circulation: Usually, tachycardiac and hypertensive
Drug Antidote: There is no specific antidote available yet.
K-Hole treatment
K-Hole treatment primarily focuses on managing the symptoms rather than the direct reversal of ketamine’s effects. Below are the vital elements of ketamine overdose treatment.
Immediate medical care: Severe cases may require airway management, oxygen supplementation, or intensive monitoring in a healthcare facility.
Symptom management: Agitation or hallucinations are treated with benzodiazepines, while hypertension and tachycardia are managed using beta-blockers or calcium channel blockers if persistent and symptomatic. Seizures can be managed with benzodiazepines and anticonvulsants like phenytoin.
Supportive measures: Vital signs are continuously monitored, IV fluids administered for hydration and blood pressure stabilization, and activated charcoal is considered for recent ingestion.
Severe complications: Respiratory depression may necessitate intubation and mechanical ventilation.
Psychiatric follow-up: After stabilization, patients may require evaluation for underlying substance use disorders or psychiatric conditions.
Urologist’ referral who may go for cystoscopy, hydrodistension and treatment with botulinum A. Drug treatment also include pentosan polysulphate and intravesical hyaluronan. If medical management fails, then substitution cystoplasty is indicated.
New treatment strategies
Once seen as a fringe party drug, ketamine – also known as “K” – has now entered the mainstream, gaining popularity as a nightlife narcotic and reports of widespread use in Hollywood. But with its rise have come warnings: several high-profile deaths, including actor Matthew Perry and drag artist The Vivienne, have sparked public concern.
To support those struggling with ketamine addiction, there is an urgent need for new treatment strategies. These include pharmacological options to address physical complications like “K cramps” (severe abdominal pain often described as excruciating) and improved understanding of how ketamine causes bladder and kidney damage.
Equally vital is improving education – both for the public and for healthcare professionals – about the risks of ketamine use and the realities of addiction.
In response to rising recreational use and recent fatalities, the UK government is reportedly considering reclassifying ketamine as a Class A drug. However, when ketamine was reclassified from Class C to Class B in 2014, use among 16–24-year-olds increased by 231%, suggesting that harsher penalties do little to curb demand.
Instead of relying on punitive measures, we must focus on expanding treatment access, reducing stigma and investing in prevention. Some studies show the urgent need for more research into what makes ketamine addictive, how to prevent its physical harms and, most importantly, how to help people recover and reclaim their lives.
If ketamine is used as antidepressant, the clinical implementation should follow strict regulatory standards and standardized protocols, as exemplified by FDA approval of intranasal esketamine for treatment-resistant depression and depressive symptoms with acute suicidal ideation in adults, always in conjunction with an oral antidepressant.[19][20].
Conflict of Interest None Declared
Authors and Contributors:
Dr. Sher Mohammad1, Dr. Hayat Khan2, Dr. Mohammad Javed Khan3, Dr. Tariq Mahmood4, Dr. Usman Ishfaq5, Dr. Muhammad Waseem Farooq Minhas6 , Dr. Emad Abo Ebeid 7,Dr.Ahmad Daoud8
- Consultant Anaesthetist(retired) STH NHS FT Sheffield
- Consultant Psychiatrist in CAMHS, Calderdale and Kirklees CAMS, South West Yorkshire NHS FT Folly Hall Mills, St. Thomas Road, Huddersfield
- Associate Professor of Anaesthesia, Khyber Teaching Hospital, Peshawar
- Assistant Professor Anaesthesia, Imran Idrees Teaching Hospital, Sialkot Medical College, Sialkot
- Trainee Anaesthetist, Imran Idrees Teaching Hospital, Sialkot Medical College, Sialkot
- Trainee Anaesthetist, Imran Idrees Teaching Hospital, Sialkot Medical College, Sialkot
- Consultant Anaesthetist(locum), Dumfries and Galloway Royal Infirmary, Scotland
- Consultant Anaesthetist(locum), Hull Teaching Hospitals, Anlaby road Hull
Correspondence Address: smyousafzai@doctors.org.uk
References:
- A Review of Ketamine Abuse and Diversion Sean Sassano-Higgins M.D., Dave Baron D.O., Grace Juarez M.D., Neevon Esmaili M.D., Mark Gold M.D. First published: 22 June 2016, https://doi.org/10.1002/da.22536
- Wood, Dan; Cottrell, Angela; Baker, Simon C.; Southgate, Jennifer; Harris, Maya; Fulford, Simon; Woodhouse, Christopher; Gillatt, David (June 2011). “Recreational ketamine: from pleasure to pain: RECREATIONAL KETAMINE”. BJU,International. 107(12): 1881–1884. doi:10.1111/j.1464-410X.2010.10031.x. PMID 21314885. S2CID 44450934.
- Deep posteromedial cortical rhythm in dissociation Sam Vesuna, ,Isaac V. Kauvar, ,Ethan Richman, Felicity Gore, Tomiko Oskotsky, Clara Sava-Segal, Liqun Luo, Robert C. Malenka, Jaimie M. Henderson, Paul Nuyujukian, Josef Parvizi & Karl Deisseroth Nature volume 586, pages87–94 (2020)
- Vincent Bonhomme 1, Audrey Vanhaudenhuyse, Athena Demertzi, Marie-Aurélie Bruno, Oceane Jaquet, Mohamed Ali Bahri, Alain Plenevaux, Melanie Boly, Pierre Boveroux, Andrea Soddu, Jean François Brichant, Pierre Maquet, Steven Laureys, PMID: 27496657, DOI: 10.1097/ALN.0000000000001275
- Synthesizing the Evidence for Ketamine and Esketamine in Treatment-Resistant Depression: An International Expert Opinion on the Available Evidence and Implementation. McIntyre RS, Rosenblat JD, Nemeroff CB, et al. The American Journal of Psychiatry. 2021;178(5):383-399. doi:10.1176/appi.ajp.2020.20081251.
- Ketamine and Rapid Antidepressant Action: New Treatments and Novel Synaptic Signaling Mechanisms. Krystal JH, Kavalali ET, Monteggia LM. Neuropsychopharmacology : Official Publication of the American College of Neuropsychopharmacology. 2024;49(1):41-50. doi:10.1038/s41386-023-01629-w.
- Pharmacotherapy: Ketamine and Esketamine. Feeney A, Papakostas GI. The Psychiatric Clinics of North America. 2023;46(2):277-290. doi:10.1016/j.psc.2023.02.003.
- Key Considerations for the Use of Ketamine and Esketamine for the Treatment of Depression: Focusing on Administration, Safety, and Tolerability. Kritzer MD, Pae CU, Masand PS. Expert Opinion on Drug Safety. 2022;21(6):725-732. doi:10.1080/14740338.2022.2069749.
- Safety and Effectiveness of NMDA Receptor Antagonists for Depression: A Multidisciplinary Review. Moore TJ, Alami A, Alexander GC, Mattison DR. Pharmacotherapy. 2022;42(7):567-579. doi:10.1002/phar.2707.
- Muetzelfeldt, L.; Kamboj, S. K.; Rees, H.; Taylor, J.; Morgan, C. J. A.; Curran, H. V. (2008-06-01). “Journey through the K-hole: Phenomenological aspects of ketamine use”. Drug and Alcohol Dependence. 95(3): 219–229. doi:10.1016/j.drugalcdep.2008.01.024. ISSN 0376-8716. PMID 18355990.
- “Ketamine”. Bristol Drug Project. Retrieved 2022-05-17.
- Stirling, John; McCoy, Lauren (December 2010). “Quantifying the psychological effects of ketamine: from euphoria to the k-hole”. Substance Use & Misuse. 45(14): 2428–2443. doi:10.3109/10826081003793912. ISSN 1532-2491. PMID 21039109. S2CID 207520095.
- 13.Rosenbaum, Steven B.; Gupta, Vikas; Palacios, Jorge L. (2022), “Ketamine”, StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 29262083, retrieved 2022-05-17
- “We Asked People About the K-Holes That Changed Their Lives”. Vice.com. 6 November 2017. Retrieved 2022-05-17.
- Curran, H V; Monaghan, L (2001-05-01). “In and out of the K-hole: a comparison of the acute and residual effects of ketamine in frequent and infrequent ketamine users”. Addiction. 96(5): 749–760. doi:10.1046/j.1360-0443.2001.96574910.x. ISSN 1360-0443. PMID 11331033.
- Zuccoli, M. L.; Muscella, A.; Fucile, C.; Carrozzino, R.; Mattioli, F.; Martelli, A.; Orengo, S. (August 2014). “Paliperidone for the Treatment of Ketamine-Induced Psychosis: A Case Report”. The International Journal of Psychiatry in Medicine. 48(2): 103–108. doi:10.2190/PM.48.2.c. ISSN 0091-2174. PMID 25377151. S2CID 37137378.
- “Ketamine: a review of use and harm”(PDF). Government UK. Advisory Council on the Misuse of Drugs and The Rt Hon Norman Baker. 2013-12-10. Retrieved 2025-06-18.
- Morgan, Celia J. A.; Curran, H. Valerie; Independent Scientific Committee on Drugs (January 2012). “Ketamine use: a review”. Addiction. 107(1): 27–38. doi:10.1111/j.1360-0443.2011.03576.x. ISSN 1360-0443. PMID 21777321.
- The Antidepressant Actions of Ketamine and Its Enantiomers. Johnston JN, Henter ID, Zarate CA. Pharmacology & Therapeutics. 2023;246:108431. doi:10.1016/j.pharmthera.2023.108431.
- FDA Orange Book. FDA Orange Book.
Image: Canva